What Happens to the Brain in Alzheimer's Disease?
On this page:
The healthy human brain contains tens of billions of neurons, which are specialized cells that process and transmit information via electrical and chemical signals. These cells send messages between different parts of the brain, and from the brain to the muscles and organs of the body. Alzheimer's disease disrupts this communication, resulting in widespread loss of brain function as many neurons stop working properly and eventually die.
Key biological processes in the brain
Most neurons have three basic parts: a cell body, multiple dendrites, and an axon.
- The cell body contains the nucleus, which houses the genetic blueprint that directs and regulates the cell’s activities.
- Dendrites are branch-like structures that extend from the cell body and collect information from other neurons.
- The axon is a cable-like structure at the end of the cell body opposite the dendrites that transmits messages to other neurons.
The function and survival of neurons depend on several key biological processes:
- Communication. Neurons are constantly in touch with neighboring brain cells. When a neuron receives signals from other neurons, it generates an electrical charge that travels down the length of its axon and releases neurotransmitter chemicals across a tiny gap called a synapse. Like a key fitting into a lock, each neurotransmitter molecule then binds to specific receptor sites on a dendrite of a nearby neuron. This process triggers chemical or electrical signals that either stimulate or inhibit activity in the neuron receiving the signal. Communication often occurs across networks of brain cells. In fact, scientists estimate that in the brain’s communications network, one neuron may have as many as 7,000 synaptic connections with other neurons. The early loss of synaptic connections is one of the main hallmarks of cognitive decline associated with Alzheimer's.
- Metabolism. Metabolism — the breaking down of chemicals and nutrients within a cell — is critical to healthy cell function and survival. To perform this function, cells require energy in the form of oxygen and glucose, which are supplied by blood circulating through the brain. The brain has one of the richest blood supplies of any organ and consumes up to 20% of the energy used by the human body — more than any other organ. In people with Alzheimer’s, there is a reduction in glucose entering the brain and also a decrease in energy production that can affect neurons due to their high energy needs.
- Repair, remodeling, and regeneration. Unlike many cells in the body, which are relatively short-lived, neurons have evolved to survive a long time, and some keep working throughout a person's lifetime. As a result, neurons must constantly maintain and repair themselves. Neurons also continuously adjust — or “remodel” — their synaptic connections depending on how much stimulation they receive from other neurons. For example, they may strengthen or weaken synaptic connections, or even break down connections with one group of neurons and build new connections with a different group. Adult brains may even generate new neurons, a process called neurogenesis. Remodeling of synaptic connections and neurogenesis are important for learning, memory, and possibly brain repair. In people with Alzheimer’s, there is some evidence suggesting decreased neurogenesis in areas of the brain involved in memory and learning.
Neurons are a major player in the central nervous system, but other cell types are also key to healthy brain function. In fact, glial cells — types of brain cells that provide physical and chemical support to neurons — are by far the most numerous cells in the brain. Glial cells come in various forms such as microglia, astrocytes, and oligodendrocytes.
Microglia protect neurons from physical and chemical damage and are responsible for clearing foreign substances and cellular debris from the brain. Astrocytes are star-shaped glial cells with important metabolic, structural, regulatory, and protective functions. Oligodendrocytes form the myelin sheath, the protective and supportive cellular insulation around axons, which are long, slender cells that send electrical signals to other parts of the body.
To carry out these roles, glial cells interact with blood vessels in the brain. Microglial cells and astrocytes are also involved in immune response in the brain. Together, glial and blood vessel cells regulate the delicate balance within the brain to ensure that it functions at its best. In recent years, an increasing amount of scientific evidence has suggested that activation of microglial and astroglia cells might play a role in brain inflammation.
How does Alzheimer’s affect the brain?
The brain typically shrinks to some degree in healthy aging, but surprisingly, does not lose neurons in large numbers. In Alzheimer’s, however, damage is widespread, as many neurons stop functioning properly, lose connections with other neurons, and eventually die. Alzheimer’s disrupts processes vital to neurons and their networks, including communication, metabolism, and repair.
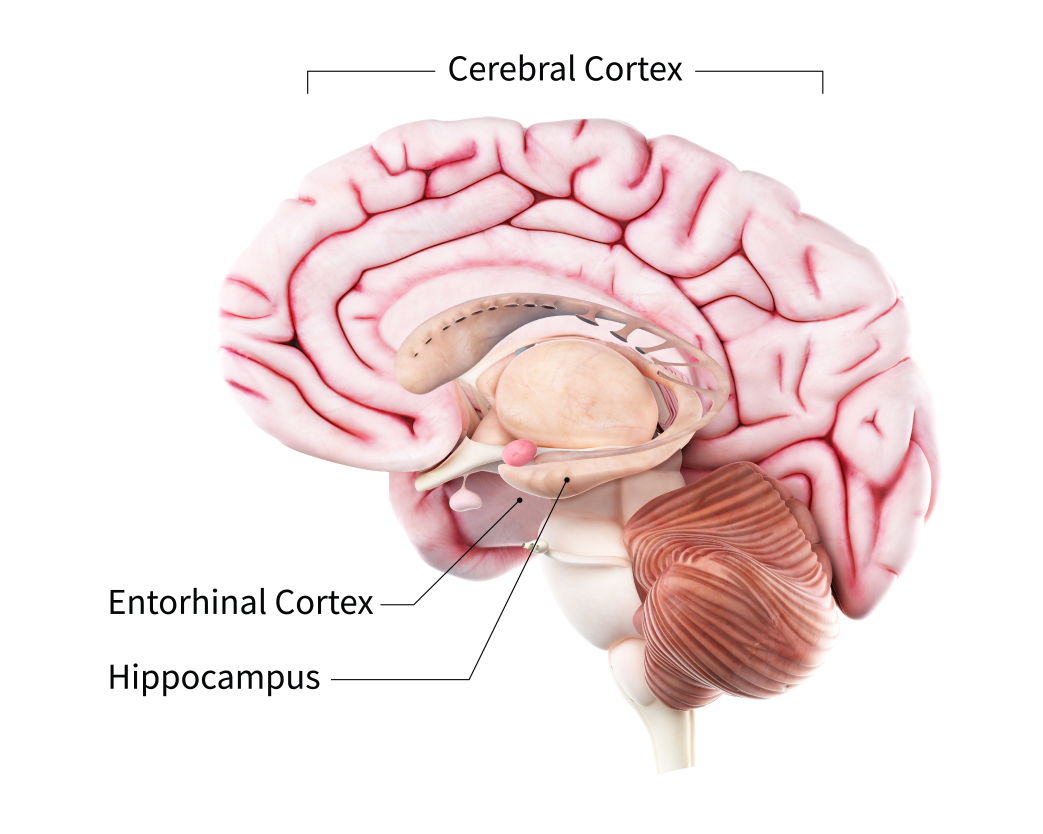
At first, Alzheimer’s usually damages the connections among neurons in parts of the brain involved in memory, including the entorhinal cortex and hippocampus. It later affects areas in the cerebral cortex responsible for language, reasoning, and social behavior. Eventually, many other areas of the brain and surrounding neurons are damaged and stop working normally. Over time, a person with Alzheimer’s gradually loses their ability to live and function independently. Ultimately, the disease is fatal.
What are the main characteristics of the brain with Alzheimer’s?
Before the early 2000s, the only sure way to know whether a person had Alzheimer’s or another form of dementia was by viewing molecular and cellular changes in brain tissue under a microscope after death. Thanks to advances in research, diagnostics including brain PET scan imaging and blood tests are now available to help doctors and researchers detect biomarkers associated with dementia in a living person, enabling more precise and earlier diagnoses. Investigations are underway to determine which changes may cause Alzheimer’s and which may be a result of the disease.
Amyloid plaques
The beta-amyloid protein involved in Alzheimer’s is formed from the breakdown of a larger protein called the amyloid precursor. It comes in several different molecular forms that collect between neurons. The beta-amyloid 42 formis thought to be especially toxic. In the Alzheimer’s brain, abnormal levels of this naturally occurring protein clump together to form plaques that disrupt cell function.
Research is evolving to better understand how, and at what stage of the disease, the various forms of beta-amyloid influence Alzheimer’s. In July 2023, the U.S. Food and Drug Administration provided its first traditional approval of the anti-amyloid drug lecanemab for its potential to reduce amyloid plaques and slow the progress of Alzheimer’s-related cognitive decline. Learn more about lecanemab and additional medications and other treatments for Alzheimer’s.
Neurofibrillary tangles
Neurofibrillary tangles are abnormal accumulations of a protein called tau that collect inside neurons. Healthy neurons are supported internally in part by structures called microtubules, which help guide nutrients and molecules from the cell body to the axon and dendrites. In healthy neurons, tau normally binds to and stabilizes microtubules. In Alzheimer’s disease, however, abnormal chemical changes cause tau to detach from microtubules and stick to other tau molecules, forming threads that eventually join to form tangles inside neurons. These tangles block the neuron’s transport system, which harms the synaptic communication between neurons.
Emerging evidence suggests that Alzheimer’s-related brain changes may result from a complex interplay among abnormal tau and beta-amyloid proteins and several other factors. It appears that abnormal tau accumulates in specific brain regions involved in memory. Beta-amyloid clumps into plaques between neurons. As the level of beta-amyloid reaches a tipping point, there is a rapid spread of tau throughout the brain.
Loss of neuronal connections and cell dysfunction
In Alzheimer’s, as neurons are injured and stop working properly throughout the brain, connections among networks of neurons may break down, and many brain regions begin to shrink. By the final stages of Alzheimer’s, this process — called brain atrophy — is widespread, resulting from significant cell death and causing the loss of brain volume.
Chronic inflammation
Research suggests that chronic inflammation may be caused by the buildup and harmful secretions of malfunctioning glial cells. Healthy glial cells help keep the brain free of debris. A type of glial cell called microglia engulfs and destroys waste and toxins in a healthy brain. When microglia fail to clear away waste, debris, and protein collections, including beta-amyloid plaques, Alzheimer’s can develop. Researchers are trying to discover the mechanisms of how and why microglia malfunction.
One study is focusing on a protein called TREM2, which is essential for proper microglial function during stress events, including neurodegenerative diseases. When TREM2 does not function normally, plaques build up between neurons. Astrocytes — another type of glial cell — are signaled to help clear the buildup of plaques and other cellular debris. Faulty microglia and astrocytes then collect around the neurons but don’t perform their debris-clearing function. They can release chemicals that cause chronic inflammation and further damage the neurons they are meant to protect.
Vascular contributions to Alzheimer’s
People with dementia sometimes simultaneously experience a number of vascular issues — problems that affect blood vessels, such as beta-amyloid deposits in brain arteries, atherosclerosis (hardening of the arteries), and mini-strokes — a combination that can negatively affect brain health. Cardiovascular problems such as high blood pressure, diabetes, and stroke can damage blood vessels and reduce the flow of oxygen and nutrients to brain tissue, resulting in compounded damage and increased risk of vascular forms of dementia.
Vascular problems may lead to reduced blood flow and oxygen to the brain, as well as a breakdown of the blood-brain barrier, which usually prevents harmful substances from getting into the brain while allowing in glucose and other necessary molecules. In a person with Alzheimer’s, disruptions to specialized transporter proteins in the blood-brain barrier may keep glucose from reaching the brain and prevent toxic beta-amyloid and tau proteins from being cleared away. This leads to inflammation, which may further worsen pathological changes in the brain. Recent studies have underscored the connection between glucose metabolism in the brain and multiple aspects of Alzheimer’s, including gender differences in risk and the severity of the disease. Researchers continue to explore potential interventions to disrupt this complicated and destructive cycle.
How do changes in the brain affect people with Alzheimer’s?
Scientists continue to unravel the complex molecular and cellular changes involved in Alzheimer’s and how they lead to the characteristic symptoms of the disease. Because the changes initially affect parts of the brain that are essential for forming new memories, memory problems are typically one of the first signs of cognitive impairment related to Alzheimer’s. Over time, additional parts of the brain are involved, causing worsening problems with thinking, reasoning, and remembering. By the later stages of the disease, damage to the brain becomes so widespread that a person can no longer communicate and is dependent on others for care.
Learn more about how Alzheimer's affects the brain and its symptoms, diagnosis, and treatment.
You may also be interested in
- Exploring different ways Alzheimer's disease is treated
- Learning about hallucinations, delusions, and paranoia
- Watching a video about brain donation
Sign up for email updates
Receive weekly tips and resources on Alzheimer's disease and related dementias from NIA's Alzheimers.gov
For more information about Alzheimer's brain changes
NIA Alzheimer’s and related Dementias Education and Referral (ADEAR) Center
800-438-4380
adear@nia.nih.gov
www.nia.nih.gov/alzheimers
The NIA ADEAR Center offers information and free print publications about Alzheimer’s and related dementias for families, caregivers, and health professionals. ADEAR Center staff answer telephone, email, and written requests and make referrals to local and national resources.
Alzheimers.gov
www.alzheimers.gov
Explore the Alzheimers.gov website for information and resources on Alzheimer’s and related dementias from across the federal government.
This content is provided by the NIH National Institute on Aging (NIA). NIA scientists and other experts review this content to ensure it is accurate and up to date.
Content reviewed:
January 19, 2024


